Author: Soma Kumari (Commentary)
Editors: Soumya Singhal and Ritwiz Sarma
Context
In December 2021, the Minister of State for Health and Family Welfare of India, Dr Bharti Praveen Pawar, announced that 13.01 lakh doctors were registered under the Indian Medical Registry (Pawar, 2021). Of these, around 80% or 10.41 lakh doctors were practising in India (National Medical Commission, n.d.). The World Health Organisation [WHO] recommends a minimum doctor-patient ratio of 1:1000 –– one doctor per 1000 patients. However, India’s doctor-patient ratio remains severely low compared to the top ten countries ranked by GDP. Presently, the ratio is 0.74:1000 for a population of 140 crores as of December 2021 (Figure 1).
Figure 1: Number of doctors per 1000 people among top ten GDP countries
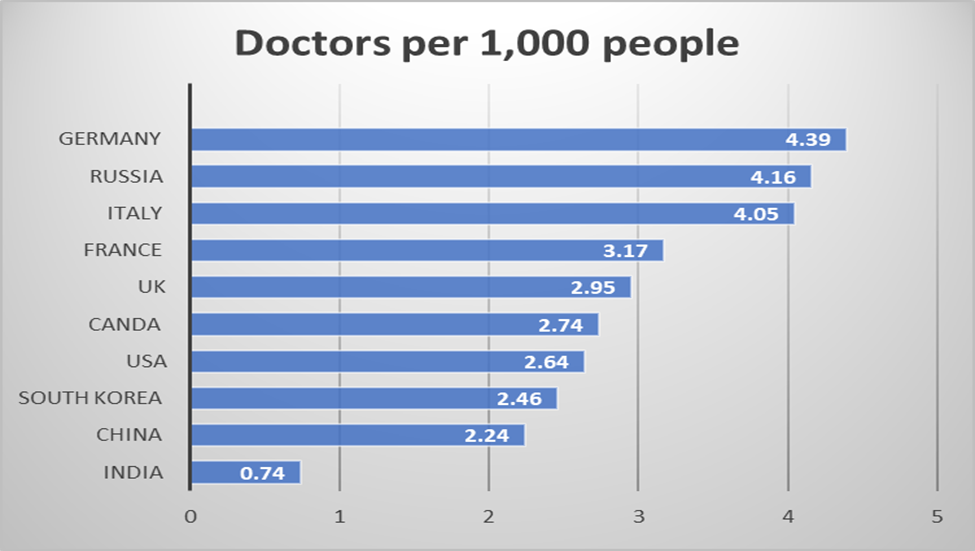
Source: India data from Karan et al. (2021). Other data from Organisation for Economic Co-operation and Development (n.d.).
An analysis of the 2018 National Health Workforce Account and Periodic Labour Force Survey by the National Sample Survey Office of 2017-2018 indicated that there are 56.7 lakh health workers in India (including allopathic doctors, nurses/midwives/dentists, among others). However, the total number of active health workers is merely 31.2 lakh (Figure 2; Karan et al., 2021).
Figure 2: Total health workers vs active health workers in India
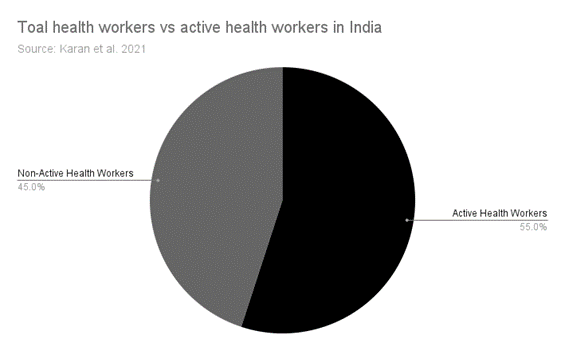 Source: Karan et al. (2021)
Source: Karan et al. (2021)
Moreover, the number of qualified doctors is estimated to be 6.75 lakhs, which accounts for just 53% of registered doctors in India. The number of uncertified health workers has risen significantly over the last two decades, with around 1.48 lakh uncertified medical practitioners or quacks currently practising (Karan et al., 2021).
India’s annual population growth rate is 0.92%, or 1.3 crores (Jankharia, 2022). The population is estimated to reach 152 crores by 2032. Even if 50,000 doctors are added annually, there will be only 11.6 lakh doctors practising by 2032, which would imply a doctor-patient ratio of 0.76:1000 (Jankharia, 2022). This skewed doctor-patient ratio will result in extremely subpar healthcare by severely overworking employees and creating a lack of qualified professionals. However, its effect on rural India will be unprecedented due to poor existing healthcare facilities.
The Ayushman Bharat Initiative was introduced in the 2019 Union Budget. The initiative suggests that the Indian population will require 1.50 lakh mid-level healthcare professionals for primary and preventive healthcare in the next 3 to 5 years (Sharma, 2019). With this structure, it will take 7-8 years to increase the supply of doctors. Until then, the system can rely upon a cadre of specially trained mid-level providers who can lead the Health and Wellness Centres known as Community Health Providers [CHPs] (Sapra, 2022). However, a WHO report states that 57% of allopathic practitioners lack medical qualifications. This figure rises to 80% in rural communities (Anand & Fan, 2016). The Indian Medical Association [IMA] has estimated that some 10-25 lakh quacks practice in India (Das, 2019).
National Medical Council- a ‘Pro-poor legislation’?
In recent years, the Indian government has attempted to address this shortage of qualified medical professionals through the National Medical Council Act [NMC], 2019. The act aims to provide high-quality medical education and adequate availability of medical professionals across the country. It further repeals the Indian Medical Council Act, 1956 [IMC Act] to dissolve the Medical Council of India [MCI].
Rural India is dependent on the Primary Health Centres and Community health centres which focus on preventive and promotive components of health care. It is intended to offer integrated curative and preventive health care to the rural population (Das & Barnwal, 2017). Within these centres, the ideal workforce is multi-layered and multi-skilled, with complementary roles delivering competent, comprehensive, continuous, and compassionate care (Reddy, 2019). The community health providers usually share the same ethnicity, language, socioeconomic status, and life experiences with the community members they serve. They either work as volunteers or on an incentive basis in association with the local health care system in rural and urban environments.
The NMC act aims to establish and empower Community Health Providers. Section 32(1) of the Act grants a limited licence “to practice medicine at mid-level as a community health provider to persons connected with a modern scientific medical profession who qualify such criteria as may be specified by the regulation.” This means the act provides a limited licence to individuals and allows them to associate with the medical profession, having met requirements set forth by the regulations to practise medicine. Further, the Act clarifies that the limited licence granted under Section 32(1) shall not exceed one-third of the total number of licensed medical practitioners. Moreover, CHPs are allowed limited scope for their medical practice. They can prescribe medicine independently, but only in primary and preventive healthcare (PRS Legislative Research, 2019). In situations related to modern medicine and surgery, they may provide treatment under the supervision of medical practitioners. Limiting the CHP licence to one-third of licensed medical practitioners can help prevent quacks from entering primary healthcare. Hence, CHPs can help remedy the shortage of trained doctors and create widespread primary healthcare access for disadvantaged sections in remote parts of India (Ministry of Health and Family Welfare, 2019).
Formalising Quackery
The provisions formalising the practice of CHPs provide an opportunity to more than 7 lakh AYUSH and other mid-level medical practitioners to improve national access to health once they hold a licence to practice allopathy. However, the IMA has raised concerns over the previously mentioned Section 32 of the NMC Act (Press Trust of India, 2019). Firstly, Section 32 does not clarify any essential criterion for granting a medical practice licence. There is no clarity on if the licence will be granted after completing bridge courses. Secondly, provisions under section 32 fail to specify the conditions and circumstances of practice. Hence, the concept and characteristics of CHPs are currently not well defined. Thirdly, Section 32(3) stipulates that CHPs can prescribe modern medicine to other domains under the supervision of medical practitioners registered under sub-section 1 of Section 32. This creates a dichotomous situation: how can a CHP registered under section 32(1) supervise another community health worker?
The NMC Act vaguely defined the term ‘Community Health Provider’. However, other terms such as ‘mid-level,’ ‘primary,’ and ‘preventive’ remain undefined. Without a well-defined structure and scope for community health providers, unqualified medical personnel would end up practising in place of qualified medical practitioners.
The Act is silent on the method for providing licences. Thus, medical malpractice can go unnoticed. Moreover, this ambiguity can risk quackery (Sharma, 2019). While the initial provision mentioned a ‘bridge course’ the new condition remains silent on providing limited licences (Bajpai, 2020).
Conclusion
The Bill intends to erode the corruption and revamp the medical education system in India. Nonetheless, it remains to be seen whether this will make access to healthcare more equitable (Honavar, 2019). The government proposes to fix the shortage of doctors by creating a new health cadre, the Community Health Providers, and leveraging them over a period of time. It is a conflicting situation because, under the supervision of someone with the same qualifications, the CHP is permitted to prescribe medications in secondary and tertiary care hospitals. This indicates that a person ‘connected’ to modern medicine is qualified to practice everywhere in India, including in rural and urban areas. They will be self-reliant and may work in emergency rooms, intensive care units, neonatal intensive care units, labour rooms, operating rooms, inpatient wards, and outpatient departments (OPDs) under the supervision of similarly competent individuals, providing inexpensive labour for corporate hospitals, which will dilute the discipline of medicine by creating an under-qualified parallel medical cadre on equal footing with traditionally qualified doctors and dilute medical ethics.
The law strictly draws the line between authorised and unauthorised doctors and prohibits unethical medical practice. The bridge course will leave an immense gap in knowledge as adequate training in medicine cannot be undergone by a student in six months or even two years. The supply-demand dynamic in the medical field cannot be resolved this way. Instead, policymakers must incentivise qualified professionals to work in rural or semi-urban areas, given the health workers’ dedication to the public health sector.
References
Anand, S., & Fan, V. (2016). The Health Workforce in India (Human Resources for Health Observer Series No. 16). World Health Organization. https://www.who.int/publications/i/item/9789241510523.
Bajpai, V. (2020). National Medical Commission Act: A Cure Worse than the Malady. Economic and Political Weekly, 55(9). https://www.epw.in/journal/2020/9/commentary/national-medical-commission-act.html.
Das, S. (2019, August 25). Will Our New Community Health Provider Please Stand Up? The Wire. https://thewire.in/health/will-our-new-community-health-provider-please-stand-up.
Das, S., & Barnwal, P. (2017). The need to train uncertified rural practitioners in India. Journal of International Medical Research, 46(1), 522–525. https://doi.org/10.1177/0300060517724948.
Honavar, S. (2019). National Medical Commission Bill, 2019 – Good intent but unmet expectations. Indian Journal of Ophthalmology, 67(8), 1259-1260. https://doi.org/10.4103/ijo.ijo_1324_19.
Jankharia, B. (2022, January 11). We don’t even know how many doctors currently practice in India. Times of India. https://timesofindia.indiatimes.com/blogs/voices/we-dont-even-know-how-many-doctors-currently-practice-in-india/.
Karan, A., Negandhi, H., Hussain, S., Zapata, T., Mairembam, D., de Graeve, H., Buchan, J., & Zodpey, S. (2021). Size, composition and distribution of health workforce in India: why, and where to invest? Human Resources for Health 19(39). https://doi.org/10.1186/s12960-021-00575-2.
Ministry of Health and Family Welfare. (2019). FAQs on National Medical Commission (NMC) Bill 2019 [press release]. Press Information Bureau. https://pib.gov.in/newsite/PrintRelease.aspx?relid=192491.
National Medical Commission. (n.d.). Indian Medical Registry Search. National Medical Commission. https://www.nmc.org.in/information-desk/indian-medical-register/.
Organisation for Economic Co-operation and Development. (n.d.). Health resources – Doctors – OECD Data. Organisation for Economic Co-operation and Development. https://data.oecd.org/healthres/doctors.htm.
Pawar, B. P. (2021). Lok Sabha – Unstarred Question Number 2299. Lok Sabha. http://164.100.24.220/loksabhaquestions/qhindi/177/AU2299.pdf
Press Trust of India. (2019, July 29). Doctors, students protest against NMC Bill. The Hindu. https://www.thehindu.com/news/national/doctors-students-protest-against-nmc-bill/article28745240.ece.
PRS Legislative Research. (n.d.). The National Medical Commission Bill. PRS India. https://prsindia.org/billtrack/the-national-medical-commission-bill-2019.
Reddy, S. (2019, August 13). Why we need community health providers. Hindustan Times. https://www.hindustantimes.com/analysis/why-we-need-community-health-providers/story-ysLykhZAHFE7FDeUCuolFP.html.
Sapra, A. (2022, January 25). The National Medical Commission Act, 2019. Community Health Providers: Legitimate or Not. India Corporate Law. https://corporate.cyrilamarchandblogs.com/2019/12/national-medical-commission-act-2019-community-health-providers-legitimatcy/.
Sharma, N. C. (2019, August 6). Mid-level Healthcare Providers An Interim Measure, Says Govt. LiveMint. https://www.livemint.com/news/india/mid-level-healthcare-providers-an-interim-measure-says-govt-1565076307070.html.



